After months of paramedic school, clinicals, internship, and training, it was official, I had been deemed competent to be the lead paramedic of an ALS ambulance. The NREMT, the State of California, and my employer had given me their blessing with full confidence that I was ready to take on whatever came my way. There was only one problem – I wasn’t.
Sure, I’d checked every box and passed every test. I had graduated from a top-tier paramedic program in the upper part of my class. Shoot, my internship preceptor had even given his stamp of approval (he wasn’t an easy one to please). Most calls I could handle well enough, but there were those few that would get me. Having done every assessment I could think of and wracking my brain for solutions, I either couldn’t figure out what was going on, or I didn’t know how to fix it. Sometimes it was both.
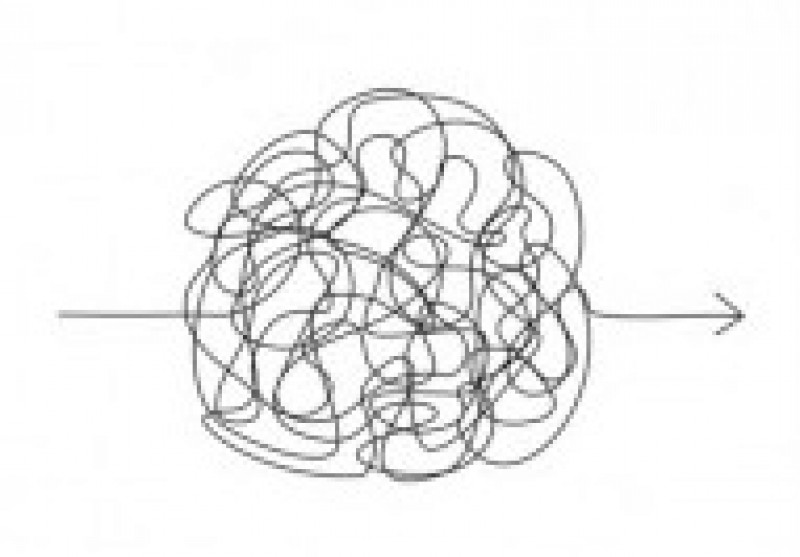
If you’ve been in EMS for more than a few months, you know what I’m talking about. Though initially terrifying, after discovering a few strategies to fall back on, these calls are now some of my favorites. For those of you who still get stumped (and who doesn’t?), I’d like to share some lessons I’ve learned from what to do when you don’t know what to do.
Beyond needing someone to drive, one of the biggest benefits of having two people on an ambulance is having a partner to fall back on. No matter who my team is, whether it’s a medic, a basic, firefighter, or ride-along, I always encourage them to let me know if they see something I’m missing. Keeping your team in the loop and giving them a voice will save you at some point or another. Guaranteed.
Another underutilized resource is our patients. Now there are times when it’s best not to let a patient know you’re unsure of the next step, but in some situations, a patient’s knowledge may be key to their treatment. This is especially true of those with complex or rare medical conditions. Seeking input from a patient isn’t a point of shame for a care provider; rather, it’s evidence of their maturity. It’s important to understand that oftentimes, it’s the patient or their loved ones who are the experts on their specific condition.
Finally, if unsure of the next step, keep the call moving forward. I distinctly remember learning this lesson. It was about halfway through my internship, and my preceptor and I were on the front porch of a patient’s home. I had a rhythm strip in hand that I couldn’t decipher. All I knew was it was uncomfortably fast, and my patient’s blood pressure was uncomfortably low. For whatever reason, medications weren’t an option, and neither was cardioversion. Try as I might, I couldn’t think what was causing the rhythm or the tenuous blood pressure. I stood there on the porch, internally deliberating about what to do, when my preceptor leaned in and asked, “What do you think about going to the hospital?”
Successfully managing a call involves moving it along toward completion. If you don’t know what to do, start working your way to the ambulance. If you are still unsure of the next treatment, why not begin driving? If you are indecisive about which medication to give, could you still start the IV? In sticky situations, I think back to what an ER physician once told me, “Air goes in. Air goes out. And blood goes round and round. If you can keep that going, most of the time, you’ll do alright.”
If you can fall back on your team, learn from your patient, and keep moving forward, I think you’ll do alright too. Best of luck.
- Dozens of courses and topics
- State-specific requirements
- We report to CAPCE in real time


