Administration of Naloxone During Emergency Medical Service Events- United States, 2018-2022
Naloxone is a fast-acting opioid antagonist that can rapidly reverse an opioid-induced overdose. In 2019, there were approximately 50,000 opioid-related overdose deaths in the United States, which marked a significant increase from prior years.1 Emergency Medical Service (EMS) providers frequently respond to overdose calls and have protocols in place for naloxone administration. A cross-sectional report found statistically significant increases in naloxone administrations during EMS activations between 2012-2016.2 Our report aims to determine the frequency of naloxone administration by licensed providers during EMS activations between 2018-2022. In addition, we aim to describe the characteristics of patients who received naloxone on EMS calls in recent years.
Data from NEMSIS, a publicly available database, was used for this analysis. NEMSIS collects data on EMS activations from over 13,000 EMS agencies across all US states and 4 territories.3 We included all EMS activations where Naloxone was administered at least once by an AEMT, EMT-intermediate, EMR, EMT, or paramedic during an emergency response between 2018 and 2022. Events where naloxone was only administered by law enforcement, lay persons, or other healthcare professionals were excluded. Facility transfers and non-emergency response activations were excluded. We calculated the rate of naloxone administration among all-cause EMS activations over the 5-year period. A sub-analysis was conducted to determine the proportion of activations for overdose-related calls that reported naloxone administration. We defined an overdose using the primary impression entered by the EMS provider. We included all activations with a primary impression of overdose, poisoning/ingestion, or opioid disorder. In addition, we compared patient demographics between 2018-2022. Chi-square tests were used to compare annual naloxone rates and patient demographics.
Table 1 compares the demographic characteristics of patients who received naloxone. The majority (65%) of EMS activations that reported naloxone administration were among calls with male patients. The average age of patients who received naloxone during the event was 46.3 years old.
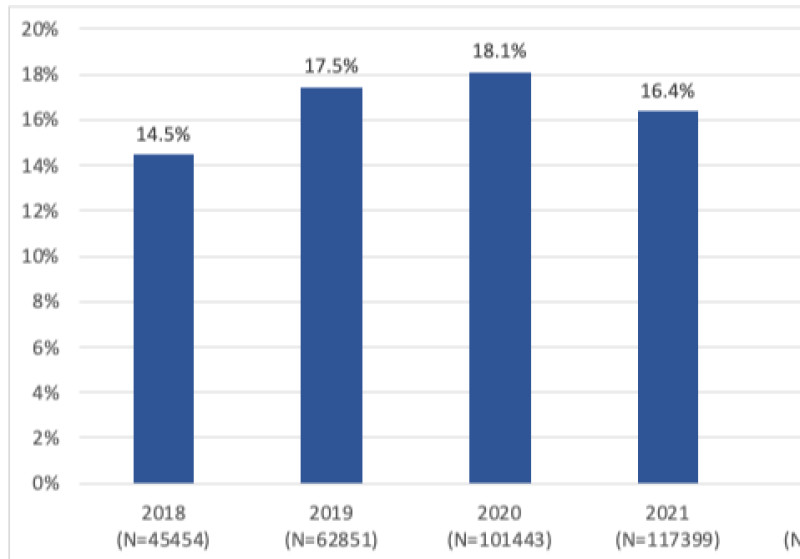
The rate of naloxone administration has significantly increased over the last 5 years. As seen in Figure 1, the rate of naloxone administrations among all EMS events increased from 200.8 administrations per 100,000 EMS activations in 2018 to 302.6 per 100,000 EMS activations in 2022 (50.7% change). Despite a substantial increase in the number of overdose-related events from 2018 to 2022, the proportion of activations for suspected overdose that reported naloxone administration remained relatively stable (Figure 2).
NEMSIS data is subject to limitations, including convenience sampling, information/selection bias, and non-random missing data, and as such, impacts the integrity of the results presented in this article.3 Despite these limitations, the data identified a substantial rise in naloxone administration and overdose-related EMS activations. Understanding trends in EMS activations is important for EMS professionals to prepare for their role adequately.
For more information on evolving EMS data and up-to-date study materials to prepare you for the NREMT exam, check out EMTprep.com! Where you can go to ensure you pass your exam – guaranteed!
Table 1: Demographic characteristics of patients with documented naloxone administration during EMS activations
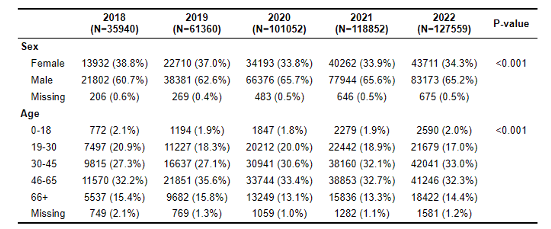
Figure 1: Rate of naloxone administration among all-cause EMS activations (p-value <0.001)
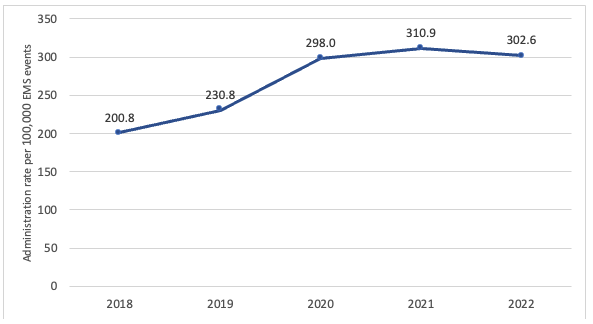
*Naloxone must have been administered by an AEMT, EMT-intermediate, EMR, EMT, or paramedic for inclusion
Figure 2: Proportion of overdose-related EMS activations reporting naloxone administration by EMS providers (p-value <0.01)
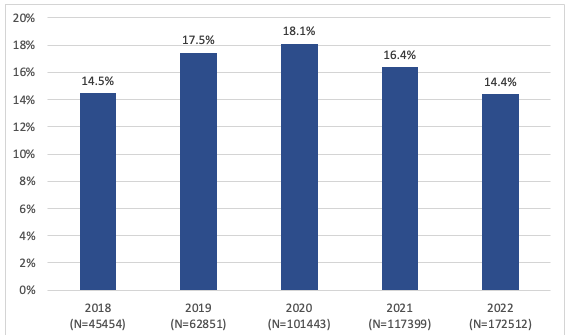
*EMS events with a primary impression of overdose, poisoning/ingestion, or opioid disorder included in the denominator
**Naloxone must have been administered by an AEMT, EMT-intermediate, EMR, EMT, or paramedic for inclusion
- 1. Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and Geographic Patterns in Drug and Synthetic Opioid Overdose Deaths — United States, 2013–2019. MMWR Morb Mortal Wkly Rep 2021;70:202–207. DOI: http://dx.doi.org/10.15585/mmwr.mm7006a4 http://dx.doi.org/10.15585/mmwr.mm7006a4
- 2. Cash RE, Kinsman J, Crowe RP, Rivard MK, Faul M, Panchal AR. Naloxone Administration Frequency During Emergency Medical Service Events — United States, 2012–2016. MMWR Morb Mortal Wkly Rep 2018;67:850–853. DOI: http://dx.doi.org/10.15585/mmwr.mm6731a2 http://dx.doi.org/10.15585/mmwr.mm6731a2
- 3. National EMS Databases. NEMSIS Public Release Research Data Set v3.4.0 2022 User Manual. Retrieved February 27th, 2024 from https://nemsis.org/wp-content/uploads/2023/04/2022-NEMSIS-RDS-340-User-Manual_v1-FINAL.pdf https://nemsis.org/wp-content/uploads/2023/04/2022-NEMSIS-RDS-340-User-Manual_v1-FINAL.pdf
- Dozens of courses and topics
- State-specific requirements
- We report to CAPCE in real time


