
As you may have learned from anatomy and physiology, carbon dioxide is a byproduct of cellular metabolism. Although it is considered waste and serves no valuable purpose for the body, it is greatly utilized in EMS and tells us a lot about what is going on in the body.
As the body reacts to different stressors, changes in carbon dioxide output occur, which can be measured using waveform capnography. End-tidal CO2 devices detect CO2 as it is exhaled from a patient's nose or mouth. These devices include a nasal cannula or a small cylinder that can be placed on the end of a tracheal tube. The end-tidal CO2 device connects to the monitor and displays a graphic representation of the patients' CO2 output in the appearance of a waveform. Capnography quantifies the amount of CO2 (in mmHg) that is exhaled over a given time (seconds). A normal waveform displays the shape of a square (sort of) and has four phases as shown below:
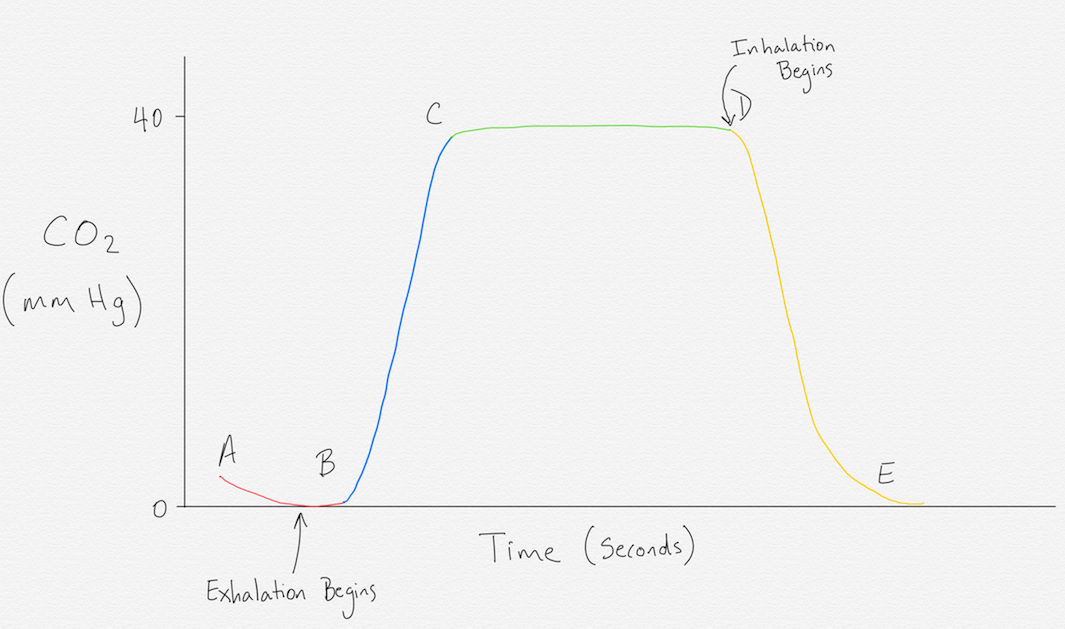
Phase I: This phase is indicated by points A and B on the diagram. This stage represents the beginning of exhalation. Since gas exchange occurs deep in the alveoli, the initial breath that is exhaled is outside air that didn’t make it to the lungs and contains no CO2. This phase is described as baseline.
Phase II: This phase is indicated by points B and C and measures the CO2 as it passes through the end-tidal device. It is normally a steep upward slope because a lot of CO2 is passing through in a short amount of time. The normal height or range of CO2 is between 35-45 mmHg.
Phase III: This phase is known as the alveolar plateau and is indicated by points C and D. It represents the emptying of the alveoli as the excretion of CO2 becomes smaller. It is the peak of CO2 exhalation.
Phase IV: This phase is indicated by points D and E and marks the point of inhalation. Atmospheric air is drawn in through the sensor containing no CO2, which is why the wave creates a sudden downward slope back to 0 mmHg and remains there until the next exhalation where it repeats itself.
Capnography is commonly used in EMS to monitor a patients’ ventilation adequacy but can be used as a tool for a number of other reasons that are valuable to an EMS provider. If intubating a patient, it is crucial to use capnography as the presence of a waveform can determine if the tube has in fact been placed in the trachea as opposed to the esophagus. Waveform capnography cannot only tell you if a patient is ventilating, but also how well they are ventilating. For example, if the waveform takes on the shape of a “shark fin”, it indicates that the patient is experiencing bronchospasms. Or if the waveform is less than 35 mmHg, it indicates that the patient is hyperventilating, and if it is greater than 45mmHg the patient is hypoventilating. Capnography can also determine the effectiveness of compressions during CPR as well as the return of spontaneous circulation (ROSC) because, in order for there to be gas exchange, blood needs to circulate to the lungs. The presence of a waveform indicates gas exchange and therefore circulation to the lungs.
Capnography is proven to be an effective tool in EMS that helps providers know if their treatments are effective; and the best part is, it’s easy to use and interpret!
- Dozens of courses and topics
- State-specific requirements
- We report to CAPCE in real time


