In this article, we will look at an overview of Acute Coronary Syndrome (ACS). We will address how to recognize it, how to treat it, and we will review some of its causes. ACS is an umbrella term that encompasses:
- Stable angina
- Unstable angina
- Myocardial infarctions.
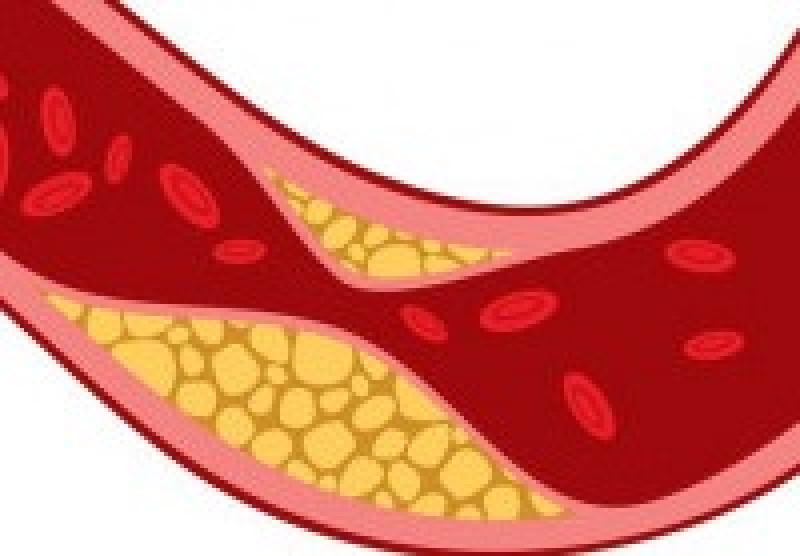
ACS is most often caused by atherosclerosis, a buildup of plaque in the coronary arteries that causes vasoconstriction and a lack of blood flow. ACS can also be caused by vasospasms which cause temporary vasoconstriction and lack of blood flow. One of the most common symptoms of ACS is chest pain, however, just because a patient has chest pain does not mean that they are suffering from ACS. There is a very long list of causes of chest pain so it is important to get a thorough assessment, history, and physical exam to determine the most likely cause.
Let’s start with the differences between stable and unstable angina. The term angina refers to the chest pain felt with cardiac tissue ischemia. The pain is caused by a narrowing of the coronary arteries either through atherosclerosis or Prinzmetal angina, a type of angina caused by vasospasms.
In Stable Angina:
- The pain is predictable typically occurring with exertion
- The pain will often last less than 15 minutes
- The pain is improved with rest and with Nitroglycerin.
- S/S: Patients may be tachycardic with the pain but will have normal to elevated blood pressure and their skin will typically be pink, warm, dry.
In Prinzmetal Angina:
- The pain is unpredictable and can occur while at rest or asleep.
- The pain is described as cyclical and resolves with medication.
In Unstable Angina:
- The pain will occur during exertion or at rest
- The pain can last longer than 15 minutes
- The pain may or may not improve with rest or Nitroglycerin.
- The episodes are also unpredictable and can come in spurts with activities that did not use to cause pain.
- The pain is typically caused by blood clots that temporarily occlude the coronary vessel which is why it can occur at rest and does not resolve with rest or Nitroglycerin.
- S/S: The patient may still be tachycardic with this type of angina, with normal to elevated blood pressure and their skin will typically be pink, warm, and dry.
This is why it is important to get a full history and find out if the patient has had similar symptoms before. You'll also want to find out if they’ve been prescribed medications for the pain, determine when the pain started, whether or not it has changed, and what they were doing when it started?
So what is the difference between angina and a "heart attack?"
Angina is caused by myocardial ischemia while a “heart attack” is caused by myocardial infarction. Infarction is tissue death caused by uncorrected ischemia. With myocardial infarction the patient may be either tachycardic or bradycardic and could be hypertensive or hypotensive, depending on where the infarction is. The patient may also be pale, cool, and diaphoretic if they are no longer able to perfuse effectively.
If the symptoms are similar how do we tell the difference between angina and an infarction?
We do a 12-lead ECG to evaluate what is going on with the heart. The 12-lead does an excellent job of revealing injury patterns. With ischemia, we will often see ST-segment depression. With infarction, we will often see ST-segment elevation. It is not uncommon with infarction to see an area of elevation with an area of depression elsewhere. This is due to further tissue ischemia around the area that is infarcted. These patients require rapid transport to a cath lab so the process of reperfusion can begin. It’s important to remember that not all myocardial infarctions show up on 12-lead ECGs. There are also non-ST elevation MIs, so just because there are no obvious ECG changes, does not mean there is no ischemia or infarction. Remember, 12-lead ECGs can change during the course of transport as you administer medications. It is important to get multiple 12-lead ECG’s so you can view any positive or negative trends with the electrical activity in your patient’s heart. This information is very valuable to the receiving hospital so be sure to have it for them whenever possible.
In summary, there are a wide array of conditions that can cause chest pain so it is important to determine where the pain is, when it started, what they were doing when it started, and what other symptoms they have with it to determine if it is cardiac or not. The amount of diagnostics we have in the field is limited so it is important to remember that we cannot rule out a cardiac issue even if the 12-lead ECG looks normal. If the patient refuses transport, it is important to thoroughly explain the risks of not transporting, determine that the patient understands and agrees to them, and document well, and encourage follow up with their cardiologist or their PCP. As Always, Follow Your Local Protocols.
References
Alaeddini J, Shirani J. Angina Pectoris. The heart.org Medscape Website. Available at: https://emedicine.medscape.com/article/150215-overview#a1.
Iqbal J, Fox KA. Epidemiological trends in acute coronary syndromes: understanding the past to predict and improve the future. Arch Med Sci. 2010;6:3-14.
www.heart.org/en/health-topics/heart-attack/angina-chest-pain
- Dozens of courses and topics
- State-specific requirements
- We report to CAPCE in real time


